How to Diagnose Celiac Disease Through Screening
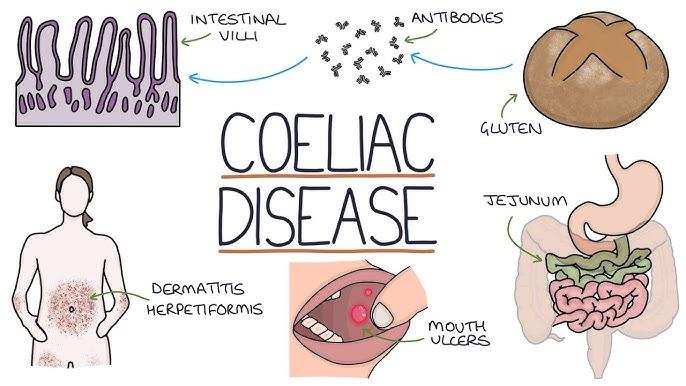
Celiac disorder is an immune condition that is triggered by gluten consumption. It affects the small intestine, leading to a variety of symptoms of the digestive system and general. It is essential to diagnose it early in order to avoid complications such as osteoporosis, malnutrition, and neurological conditions. Diagnosing celiac disease requires multiple steps, ranging from blood tests to confirmation biopsies.
1. Identifying Symptoms and Risk Factors
In the initial screening phase, medical professionals evaluate the signs or risk elements. The most common signs are:
Constipation or diarrhea that is chronic
Abdominal discomfort and the sensation of bloating
Insomnia and fatigue
Unexplained weight loss
Skin rash (dermatitis herpetiformis)
Anemia due to iron deficiency
Nervous or joint pain
Individuals at high risk, such as those who have a family history of celiac disease or type 1 diabetes, or any other autoimmune diseases, are usually advised to undergo screening.
2. Blood Tests for Celiac Disease
The initial step of celiac disease screening is to conduct the use of serological (blood) testing to identify antibodies that could indicate that gluten is the cause of the immune response. The most frequently used tests include:
Tissue Transglutaminase antibody (tTG-IgA and TTG-IgG): The most accurate test, having high sensitivity, and precision for celiac disease.
Edomysial Antibody (EMA-IgA): Highly specific, but not widely utilized due to its complexity.
Deamidated Gliadin peptide (DGP-IgA as well as DGP-IgG): Useful in those suffering from IgA deficiency.
Complete Serum IgA: Ensures accurate test results, as IgA deficiencies can impact reliability.
Notification Important: These tests should be conducted while the person is eating gluten. A gluten-free diet prior to the testing could result in false negative results.
3. Genetic Testing for Celiac Disease
Genetic tests can help rule out celiac disease. It detects that there are HLA-DQ2 as well as HLADQ8 genes that are linked with the disease. But, having these genes doesn't mean you have celiac disease. In fact, only 3 percent of those with these genes actually suffer from the condition.
4. Confirmatory Small Intestine Biopsy
If blood tests show celiac disease, a small intestine biopsy can be done using the upper endoscopy. This is the process of placing a thin tube and cameras into the small intestine to take tissue samples. The villi of the intestine are damaged (flattening or atrophy), which is a sign of celiac disease.
5. Non-Invasive Screening Alternatives
For those who are unable or unwilling to undergo biopsy, alternative ways to diagnose are:
Capsule Endoscopy: The tiny camera within the pill records pictures of the small intestine.
Fecal as well as Saliva tests: These are still being investigated and are not frequently used to determine diagnosis.
6. Diagnosis and Next Steps
Once diagnosed, gluten allergy testing illness is controlled by eliminating gluten in foods, medications and supplements. Regular visits to a healthcare doctor ensure relief from symptoms and also check for nutritional deficiencies.
Conclusion
Testing for celiac disease is the use of tests for blood, genetic testing and, if needed, the biopsy of your intestine. The early detection of celiac disease helps avoid chronic complications and enhances your quality of life. If you suspect that you have gluten intolerance or celiac disease, make an appointment with a doctor for a thorough examination and test
